Tradition tells us that a bad burn can be healed with honey. I’m sure you’ve heard this already. but what is less known is that this is a practice also supported by in vitro studies, laboratory experiments and clinical trials, published in the specialized literature. Compared to other modern dressings for wounds (for example nanocrystalline silver dressings) honey has the vastest amount of scientific evidence that proves its efficiency. Yet, people are still reluctant.
Honey has anti-infectious and anti-inflammatory properties and a favorable effect on wound regeneration. I know that lately we have all heard about the magical powers of manuka honey, but the truth is that any type of honey is good to treat wounds and burns. What makes manuka honey that special when it comes to wounds, is that its content of methylglyoxal (MGO) helps in killing even the most resistant bacteria that would keep a wound from healing.
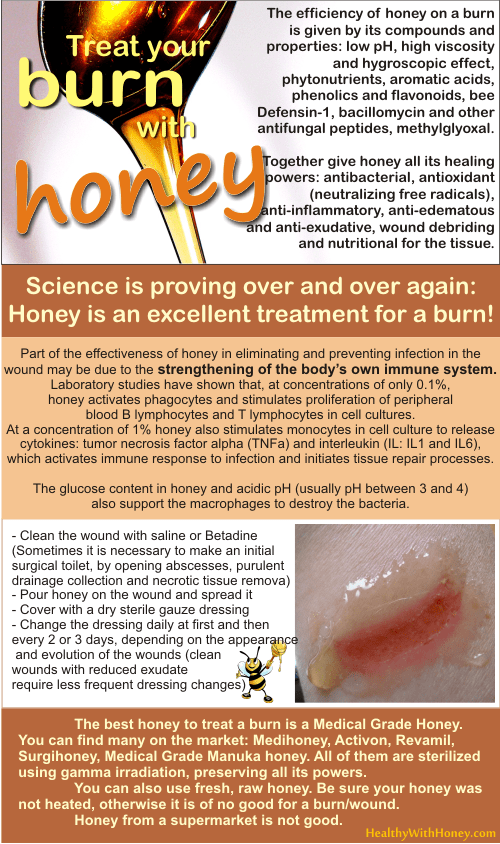
To a higher degree any type of honey can heal a burn, as long as it is indeed honey, raw, unprocessed honey (see What is processed honey). Of course the best is one that has been first sterilized (using gamma radiation), as it is the case with every medical grade honey available on the market (see surgihoney, medihoney, revamil, activon) which eliminates the possibility of any type of microorganisms or spores that could be present.
All undertaken studies have evidenced honey’s properties and effects on burns: anti-infectious, anti-inflammatory, antiexudative, antioxidant, wound healing, wound debriding and nutritional.
Factors that contribute to honey healing burns
There are several factors that together contribute to healing burns: high concentration of sugars (and from here its high osmotic concentration and hygroscopic power), low pH, glocose oxydase enzyme which lead to hydrogen peroxide formation, other antibacterial substances like methylglyoxal (in manuka honey and berringa honey), Bee-defensin-1, melanoidins, phytonutrients and other, yet unidentified, compounds.
Honey is anti-infectious
Honey has proven to have a broad-spectrum anti-infectious action against at least 80 species of micro-organisms including:
– Gram positive and Gram negative bacteria, aerobes and anaerobes,
– some fungal species of Aspergillus and Penicillium and all the common dermatophytes, including types of bacteria multi- resistant to antibiotics, such as Pseudomonas, Acinetobacter, methicillin-resistant (MRSA) and coagulase-negative Staphylococcus aureus (with a minimum inhibitory concentration (MIC) generally below 10%, usually inferior to that present in wounds where the honey was applied).
Bang LM and colleagues showed in 2003 that honey is fully effective against antibiotic-resistant bacteria. Over time there was no loss of bacterial sensibility to honey and no appearance of bacteria resistant mutants.
Honey was efficient where antibiotics failed, because it is effectively including aggregated bacteria in biofilms, a situation where antibiotics and silver dressings proved ineffective.
The antibacterial properties of honey are supported either by the hydrogene peroxide properties, or by other substances such as methylglyoxal and phytonutrients.
Read more about What gives honey its antimicrobial power?
Hydrogen peroxide.
Honey bees add some enzymes (secreted by their hypopharyngeal gland) into the nectar they collect from the flowers in order to make honey. It is the case of the enzyme “glucose oxidase”. As this name suggests, this enzyme oxidase the glucose and turns into gluconolactone and hydrogen peroxide.
Hydrogen peroxide (H2O2) is a disinfectant agent used in our medicinal world and present in our body. It is involved in many cell types as a stimulus for cell proliferation, for the growth of fibroblasts and epithelial cells to repair damage, for the development of new capillaries in damaged tissue, as part of the normal inflammatory response to injury or infection.
There is a thin line between too much and too low concentrations on hydrogen peroxide in stimulating wound healing. At high concentration the production of oxygen radicals would lead to more tissue damage. That is why using pure peroxide oxidation bought from a drug store is not recommended any more, not even for sterilizing the wound.
If you have crystallized honey, be sure you heat it at a temperature below 40°C. Overheating honey should be avoided, since the enzyme glucose oxidase in honey that produces hydrogen peroxide is easily inactivated by heat. Such a honey will be of no use on a burn.
Methylglyoxal (in Manuka honey and Berringa honey from New Zealand).
After neutralizing the enzyme in honey responsible for the formation of hydrogen peroxide, this MGO is the substance that has powerful antimicrobial effects and fight infections on a wound (burn).
Honey is anti-inflammatory, anti-edematous and anti-exudative
Studying the possible mechanisms of honey’s inflammatory activity researchers listed:
– inhibition of complement,
– inhibition of nitric oxide production by macrophages,
– inactivation and suppression of reactive oxygen species (ROS) by phagocytes,
– decrease of thermal injuryinduced oxidative stress by controlling free radicals that are formed in the burn wound
– apalbumina-1, a protein secreted by bees.
The anti-inflammatory effect and suppression of ROS, which overstimulate fibroblasts, lead to a reduction of fibrosis and hypertrophic scarring.
To make a comparison, synthetic anti-inflammatory drugs do not promote wound healing (non-steroidal anti-inflammatory substances are cytotoxic drugs, and corticosteroids inhibit the growth of epithelium).
Considering its anti-inflammatory effect, honey is as effective as prednisolone in a trial on induced colitis in rats, and a statistically significant (p <0.001) reduction of postoperative peritoneal adhesions on the cecum and ileum in another trial on rats.
Honey is antioxidant
Honey has antioxidant activity by controlling free radicals and ROS (reactive oxygen species). The ROS act as messengers that amplify the inflammatory response and this process can be blocked by antioxidant substances present in honey at a high level.
On the other hand, ROS produced by phagocytes in inflamed tissues activate proteases that are normally inactive and their activated forms digest extracellular matrix and cell growth factors that are essential for tissue repair.
Read more about Natural antioxidants in honey. Do we really need antioxidant supplements?
Honey is hygroscopic
This means that honey draws moisture out of the environment.
Honey has a high viscosity and the capacity of drawing humidity from the environment by osmosis. Thus creates a physical barrier and moist local environment, which promotes healing. It is known that wounds heal faster when kept moist as opposed to when they are left to dry out and form a scab.
A moist environment ensures the growth of epithelial cells, the contraction of fibroblasts to approach the wound edges, as well as non-adherence of dressings to the wound, leading to easy and painless dressing changes, without the risk of breaking newly formed epithelium.
This means lifting and removing waste and debris from the wound, which may even eliminate the need for surgical debridement.
Dressing changes will be painless with no risk of damage or tearing of newly formed tissue.
Also, a local environment allows the protein-digesting enzymes in the wound tissues to work and loosen any scab and dead tissue.
What are the enzymes present in raw honey? Why are they important?
In order to form hydrogen peroxide the enzyme glucose oxidase needs water. Raw honey contains only about 17% water, and almost entirely bound by carbohydrates, not free so the enzyme could use it. That is why hydrogene peroxide is found only in tiny amount, if any, in raw honey.
But honey is able to draw water from the environment, from the air or from a wound. Small amounts of exudates from the wound would be used by the enzyme to oxidase the glucose in honey into small amounts of gluconic acid and hydrogen peroxide. Enough to promote healing and not damage the tissues.
The amount of hydrogen peroxide found inside the wound depends on the balance between its production rate (by the glucose oxidase) and the rate of destruction (plasma enzymes such as catalase and glutathione peroxidase).
Studies have shown, ever since 1919, that diluted honey activates its antibacterial properties. The maximum accumulated hydrogen peroxide (1-2 mmol/L) (after Cooper R, 1999) is found in diluted honey solutions at concentrations between 30% and 50% (v/v), at least 50% of the maximum level at concentrations between 15-67% (v/v).
Honey has a wound debriding action
It activates plasminogen and increases plasmin enzyme activity, which lyses fibrin attaching slough, by suppression of the macrophage plasminogen activation inhibitor. Plasmin digests fibrin, which attaches debris on wound surface, but does not digest collagen extracellular matrix, which is necessary for tissue repair.
Honey is nutritional
Tissues heal faster if they are supplied with nutrients.
Honey has a nutritional action in the wound, indirectly through osmotic flow of lymph, which brings nutrients needed for healing, but also directly through an intake of easily metabolized carbohydrates, amino acids, vitamins and minerals.
Scientists say that “honey provides glucose support for epithelial cells, leukocytes and for the process of glycolysis. The epithelial cells require a reserve of carbohydrates for energy migration over the wound surface to restore epithelial sheath. Leukocytes create the respiratory (oxidative) burst that produces hydrogen peroxide, which is the dominant component of macrophages antibacterial activity. Finally, glycolysis is the major mechanism of energy production by macrophages, allowing them to function in damaged tissues and exudates where oxygen is often limited.”
Honey has a high acidity
The acidity of honey (a pH of usually less than 4) contributes to the antibacterial action of macrophages, since an acidic pH inside the vacuole is involved in destroying the ingested bacteria.
The low acidity prevents the appearance of the non-ionized histotoxic form of ammonia, resulting from the action of urease (from urease-producing microorganisms) on urea in the extracellular fluid. In an acidic medium, ammonia (NH3) is converted to ionized, nontoxic, ammonium ion (NH4+).
The acidification of the wound increases oxygen intake and pO2 on wound surface thus improving the rate of healing.
High carbohydrate levels conferred by honey can be used by bacteria in preference to amino acids in the serum and dead cells, thus creating lactic acid instead of ammonia, various amines and sulfur compounds (the cause of malodour [the dead rabbit smell] in burns).
What honey is the best to treat a burn?
Any type of medical grade honey is the best honey to heal a wound or a burn. That is because it was sterilized using gamma radiation, this removing any possible spores or microbes, while still preserving its medicinal properties. Some of them are made of manuka, some are made from selected medicinal plants in greenhouses. They are all very good.
There are plenty of them on the market: Medical Grade Manuka Honey, Medihoney, Activon, Revamil, Surgihoney.
If you don’t have any in the house and cannot wait to buy it, then use any type of raw honey. Make sure it was not heated (to be filtered) because the enzyme glucose oxidase which is present in a fresh honey and the one that produces hydrogen peroxide, an important factor in healing the burn, is easily inactivated by heat. It will be useless.
Do not use honey bought from a regular supermarket, especially if the label says: “pure honey”. That honey was so purified that it contains nothing more than sugars in it.
==========
References:
Up-to-date use of honey for burns treatment, A. Zbuchea, 2014
Picture source forum.facmedicine.com