Again about how good it is, right? Can manuka honey kill Pseudomonas aeruginosa or Burkholderia spp, both involved in cystic fibrosis and chronic granulomatosis? Well, there is good news on this.
We heard manuka honey is the best honey. Funny enough, the thing that most people know is that it kills superbugs, like Staphylococcus aureus or Helicobacter pylori, and know less that it is excellent for any type of wound or burn – which is its main health benefit.
The fact that it is an excellent antibacterial agent is confirmed buy numerous studies, its UMF grades and high price. Well, the price doesn’t necessarily imply good quality, though in this case, it is a mark of value.
On the other hand, there is a well-known tendency of pathogenic bacteria to acquire resistance to conventional antibiotics, thus new strategies of antimicrobial treatment must be sought. Recently conventional medicine turned to natural products and tried to combine them with synthetic drugs to enhance their effect. It happens with manuka honey as well, given its proved antibiotic power, lack of side-effects and capacity of not causing resistance.
Manuka honey – breakthrough treatment for cystic fibrosis patients
How is this possible? Thanks to the powerful antimicrobial effect of manuka honey. This natural product can be used as an antibiotic alternative for the treatment of antimicrobial resistant respiratory infections, particularly deadly bacteria found in Cystic Fibrosis infections.
This is what a study from 2015, conducted by Rowena Jenkins from the Department of Biomedical Sciences, Cardiff School of Health Sciences, UK, showed in the study “A demonstration of the susceptibility of clinical isolates obtained from cystic fibrosis patients to manuka honey.”
Two bacteria are known to be responsible for causing serious and chronic respiratory infections in vulnerable patients, especially those with underlying conditions such as cystic fibrosis or chronic granulomatous disease: Pseudomonas aeruginosa and Burkholderia spp. (Both bacteria also implicated in wound infections).
Why are these 2 bacteria bad in cystic fibrosis and chronic granulomatosis?
Because chronic colonisation of the lungs of cystic fibrosis patients by mucoid strains of P. aeruginosa and Burkholderia is associated with deteriorating lung function which results in a poor prognosis.
Why is Pseudomonas aeruginosa so difficult to kill?
Because its outer membrane has a low permeability, which restricts antibiotics from penetrating into the bacterium. Compared to E. coli, the membrane of P. aeruginosa is 12-100 times less permeable (Nicas and Hancock 1983).
As a result, it is resistant to many antibiotics.
To this condition we may add the gene mutation and gene acquisition which will confer resistance to a range of antibiotics including β-lactams, aminoglycosides and fluoroquinolones, making these strains more difficult to inhibit.
Why is Burkholderia difficult to kill?
Because they are widely distributed throughout the environment: in soil, water, insects and plants as well as from humans, where they will have been exposed to many antimicrobial compounds (Compant et al. 2008). These bacteria have reached the point where some of the strains utilize penicillin as a sole carbon source (Vermis et al. 2003) and that others survive in solutions of the hospital disinfectant, such as chlorhexidine (Heo et al. 2008)! While other strains are simply resistant to many available antibiotics (Mahenthiralingam et al. 2005).
Both of these bacteria are prolific biofilm formers, especially in cystic fibrosis patients, where up to 1000 times the concentration of antibiotic is needed to kill the equivalent planktonic cell (Mah and O’Toole 2001). Added to the natural resistance of these bacteria, this makes these tenacious bacteria a real therapeutic challenge.
Can manuka honey kill Pseudomonas aeruginosa and Burkholderia spp?
Yes, this was demonstrated on 22 strains of B. cepacia (Cooper et al. 2000) and of 17 strains of P. aeruginosa
isolated from burns (Cooper et al. 2002), using raw non-medical-grade (non-sterilised) honey samples.
But these days, when we talk about manuka honey used to treat burns and hard-to-heal wounds, only medical grade manuka honey is used. This is sterilized manuka honey, made by gamma-radiation. The study mentioned above used sterile medical-grade Comvita manuka honey 18+ to test the susceptibility of 111 clinical isolates of P. aeruginosa and B. cepacia, collected from a range of infections, to manuka honey alone and in combination with currently used antibiotics.
The results for manuka honey alone, showed that Burkholderia cepacia demonstrated a higher susceptibility to manuka honey than Pseudomonas aeruginosa [previously had been shown that B. cepacia is more resistant
to antibiotics than P. aeruginosa (Wilkinson and Pitt 1995)].
To show how manuka honey works in combination with antibiotics, scientists chose tobramycin and colistin because these drugs are licensed for use as inhaled antibiotics in treating chronic respiratory infections in cystic fibrosis, a rather new form of treatment. The results showed the following:
– manuka honey + colistin worked in synergy for both P. aeruginosa isolates and one of the B. cepacia isolates.
– manuka honey + tobramycin worked in synergy against one of the P. aeruginosa species.
As a result it is recommended that honey combined with selected antibiotics to be developed into an inhalation compound for use in patients with respiratory infections.
All the findings of this study, which analyzed the action of gamma-radiated manuka honey were consistent with previous data obtained in earlier studies made with raw manuka honey (Cooper et al. 2000, 2002). It also showed that the susceptibility of respiratory isolates to honey did not differ markedly from that of wound isolates.
Manuka honey at relatively low concentrations inhibits the growth of clinical cystic fibrosis isolates of both P. aeruginosa and B. cepacia and acts synergistically with two pertinent antibiotics (tobramycin and colistin ).
*************
You may also be interested in:
• What about manuka honey’s strong antibacterial properties? What makes it so special?
• Is honey good for ulcer? Does manuka honey kill Helicobacter pylori?
• What kills Staphylococcus aureus? Does manuka honey kill MRSA?
• I want to buy manuka honey. What is UMF 16+, MGO 400+, Active?
• Is Manuka Honey safe to eat?
• What is UMF and how to read the label of manuka honey
If you had any experience with manuka honey, please share your story here. We all need to learn from each other’s experience. We salute all the scientists who are working hard to uncover the benefits of manuka honey to us all, yet we still need to learn also from experience and let them know what we have discovered ourselves.
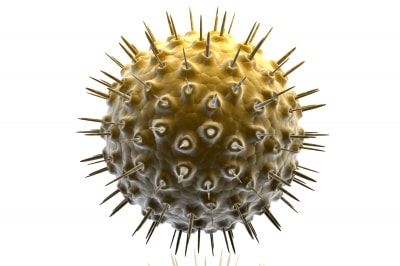
Featured picture background by Y_tambe – Y_tambe’s file, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=49535.